At the end of 2018, our hospital – the SS. Antonio e Biagio e Cesare Arrigo hospital (AO AL) in the city of Alessandria, in northern Italy – established a multi-year strategic plan based on the implementation of lean projects in different areas of the organization. As part of this effort, a team of internal lean coaches was created, tasked with developing the lean capabilities of the hospital’s employees and supporting the development of improvement initiatives coming both from the front line and the management team.
The Covid-19 pandemic presented us with a huge challenge. On March 6th, the regional government of the Piedmont region chose the microbiology laboratory in our hospital for the processing of swab tests for the detection of Covid-19 infections. We were aware of the huge spike in demand we were going to experience and realized we had to quickly reorganize our laboratory.
We decided, therefore, to create a dedicated space for the pre-analytical phase of testing, open seven days a week. We completely reengineered our production process to meet the growing demand and guarantee a quick analysis of samples coming from hospitalized patients, but also from patients from the area our laboratory is responsible for (as well as those that couldn’t be processed by other nearby heath authorities and that the regional government asked us to take).
Not only did we have to increase our capacity, but we also had to analyze the process in detail to identify inefficiencies.
Here you can see the different steps in our process:


The original process, which was almost entirely manual, required a lot of effort by the administrative staff, especially in the initial steps of cross-referencing and registration, to upload paper-based requests onto the lab’s IT system – with the high risk of making mistakes.
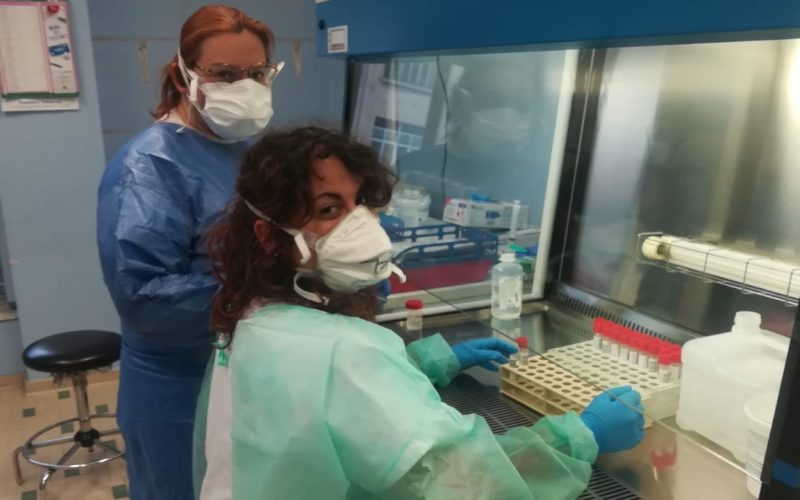
As far as the pre-analytical phase is concerned, we also created a dedicated team of technicians and biologists and managed to find a room that could be used exclusively for aliquoting samples in secondary test tubes to essentially pre-process the swabs and then assign them to the available machines. This is when the pre-analytical phase is complete.

Samples are distributed to two types of machines, each with its own cycle duration and capacity (to start the cobas machine, for example, means waiting to have 94 samples to test – lest we waste reagents), based on where they come from and on priority.

Over the first few weeks of the Covid-19 crisis, the reorganization of the process led to an exponential increase in the number of swab tests we can process – as shown in the graphic below.

Despite the increased activity, the laboratory has been able to gradually reduce its turn-around time (TAT), except for the week of March 16th, when we didn’t receive the reagents that we needed to process the samples.

We are also planning the implementation of another countermeasure that aims to speed up the classification of patients in our Emergency Room: the instalment of the GeneXpert machine, which is currently capable of processing between two and four samples every 45 minutes. Placing the machine in the ER and making it directly available to ER staff would enable a 24/7 activity cycle and the immediate identification of Covid-19 cases.